- TOP
-
What is
immunity? -
How to keep
the immune system? -
L. lactis Plasma
- What is L. lactis Plasma?
- Effects of L. lactis Plasma
-
Academic Reports and
External
Announcements

Aging, stress, exercise, and sleep habits are known to be associated with decreased immunity.
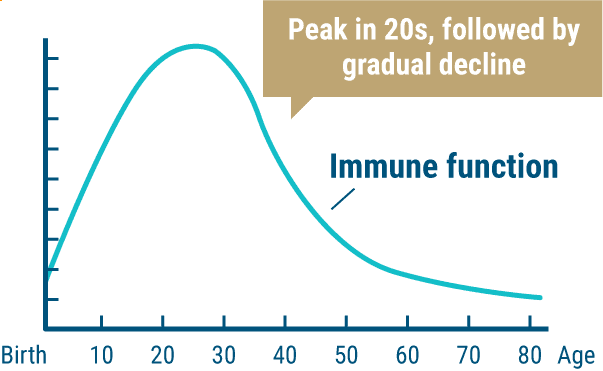
01Aging and Immunity
After birth, a person builds up their immunity by being exposed to the outside environment. Immune function peaks in your 20s and gradually declines with age.
Decline in immune function due to aging
Reference: "Mechanisms of the Body and
Immunity," Japan
Jitsugyo Publishing Co.
02Stress and Immunity
Chronic stress can lower immunity. Stress, when moderate, has a positive effect, but when it becomes excessive, it can rapidly cause health problems.
03Sleep and Immunity
Sleep time is said to be on the decrease compared to the past. And it has been reported that the less you sleep well, the more likely you are to catch a cold.
This suggests that there is a connection between the immune system, which protects against enemies from the outside, and sleep.
Relationship between susceptibility to colds
and getting sound sleep
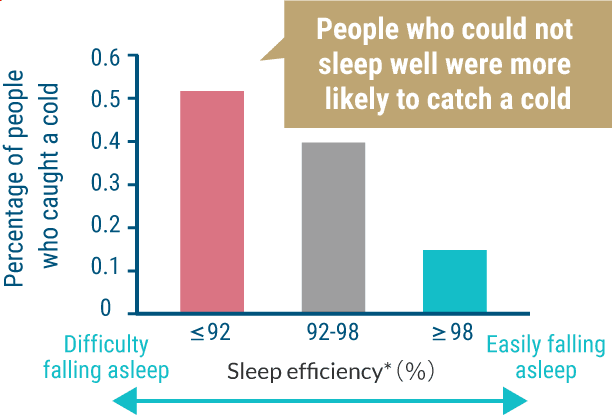
*Efficiency from getting into bed to actually falling asleep
Partially modified from Cohen, Sheldon, et al. "Sleep habits and susceptibility to the common cold." Archives of internal medicine, 169.1 (2009): 62-67
04Exercise and Immunity
It is known that intense exercise temporarily reduces immune function. This phenomenon is known as the "open window" and can be a major problem for exercisers (see left figure below).
In fact, top athletes and those who engage in strenuous exercise have been reported to have a higher incidence of infections than the general population (see right figure below).
Temporary immunosuppression
due to strenuous exercise
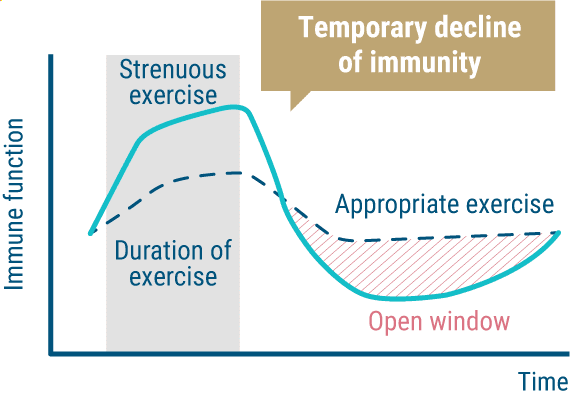
Reference: partially modified from "Will I stop getting colds
if I exercise?", Journal of the Humanities, Vol 57 (2011.3)
Incidence rate of colds after hard training
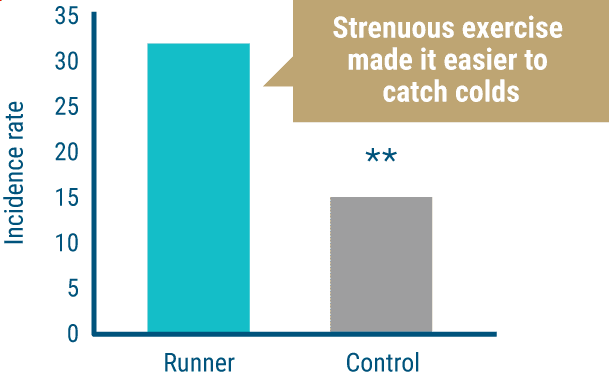
** indicates statistically significant with P<0.01
Source: Med Sci Sports Exerc. 26: 128-139 (1994)
05Obesity and Immunity
At first glance, obesity and immunity may seem to have little to do with each other. Actually, they are closely related, and it has been found that people with obesity, especially visceral-fat obesity, are more likely to have lowered immune function. We therefore asked Dr. Yoshihiro Kitamura, Deputy Director of the Center for Medical Education at Nippon Medical School, about the relationship between obesity and immunity.
What is the relationship between obesity and immunity?
In recent years, the relationship between fat-especially visceral fat-and immunity has been the focus of much attention. In the bodies of people with visceral-fat obesity, the balance of hormones secreted by visceral adipose tissue is disturbed, resulting in a state of persistent systemic inflammation, or "chronic inflammation". This chronic inflammation leads to a decline in immune function, which in turn leads to infections becoming severe and other problems.
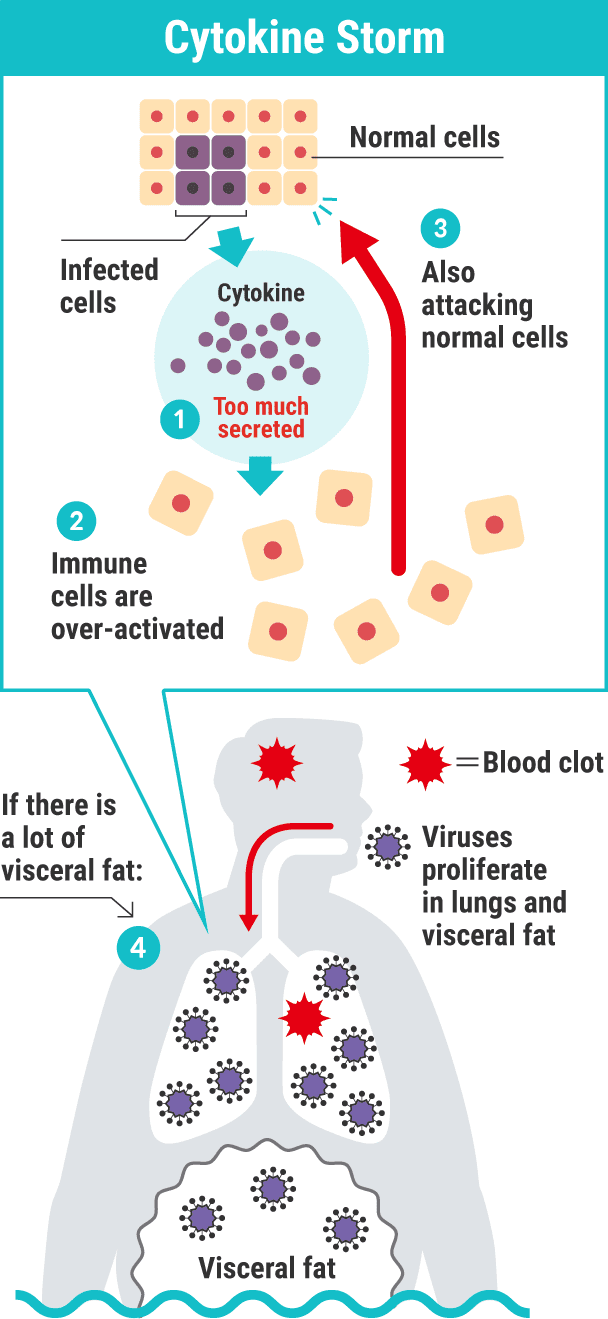
You say that obesity is an inflammatory condition, but that's hard to visualize...
Unlike so-called acute inflammation, in which the affected area swells and turns red when a foreign enemy such as bacteria or a virus invades, chronic inflammation is a state in which the immune system is in constant battle-mode even though there is no enemy from the outside. The immune system, which was originally supposed to fight enemies from the outside, is malfunctioning in a runaway state even though there are no enemies present, so it's in a doubly-bad state because it's not only weaker when it comes time to fight outside enemies but it also damages your own normal cells. So, conversely, it can be said that eliminating the inflammatory condition of obesity leads to an increase in immunity.
What are the actual dangers when bacterial and viral infections occur in people with obesity?
In a report on COVID-19, it was found that "people with obesity have a higher rate of ICU admission and a higher rate of severe illness than people of normal weight."
When a person with obesity is infected with the virus, chronic inflammation within the visceral adipose tissue rapidly worsens. Cytokines, proteins that activate immune cells, are released explosively, and as I mentioned earlier, the immune system goes into a runaway state. This is called a cytokine storm. Overly activated immune cells attack your own normal cells as well, leading to more severe infections.
We often hear that obesity causes lifestyle-related diseases, but I never knew that it also lowers immunity.
You become more susceptible to infections.
That's right. But in addition to fighting bacteria and viruses, the immune system also plays an important role in repairing aging cells and tissue damage. When immune function is degraded or out of control due to chronic inflammation, this role is also compromised. Blood vessels throughout the body also age more rapidly, and your face looks older, with more wrinkles and spots than normal for your age.
That's frightening... So immunity is also important for anti-aging!
Yes it is. As we have explained, visceral fat and immunity affect each
other, so optimizing them at the same time is quite a powerful technique
for better health. It is very important to improve eating habits and to incorporate an appropriate level of exercise.
Many people are concerned about unbalanced diets and lack of exercise due to remote work. Let's start by improving eating habits, and begin light exercise such as walking and calisthenics! Sometimes, a good supplement focused on visceral fat and immunity care can help the body to resist both infections and
lifestyle-related diseases.

 Kirin is studying
Kirin is studying
the effects of
continuous
exercise on immune function

In collaboration with Juntendo University, Kirin conducted a study on the effects of continuous exercise on the immune system. The activity of plasmacytoid dendritic cells (pDCs), the "leaders" of the immune system, was measured in 22 university students belonging to an athletic club during a 14-day period of continuous exercise. The results revealed that pDC activity was significantly lower after exercise compared to before. The results of this study also suggest that strenuous exercise causes a lowering of immunity.
Testing schedule

Effect on immune function
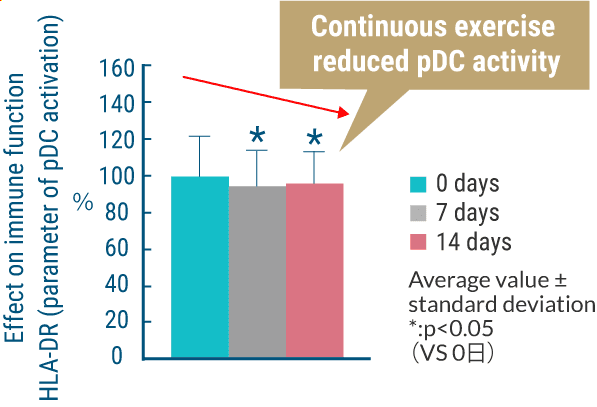
Source: 72nd Annual Meeting of the Japan Society
of Physical Fitness and Sports Medicine (2017)


Commentary and supervision:
Dr. Yoshihiro Kitamura
Deputy Director of the Center for Medical Education,
Nippon Medical School,
and Specially Appointed Professor.
Doctor of Medicine